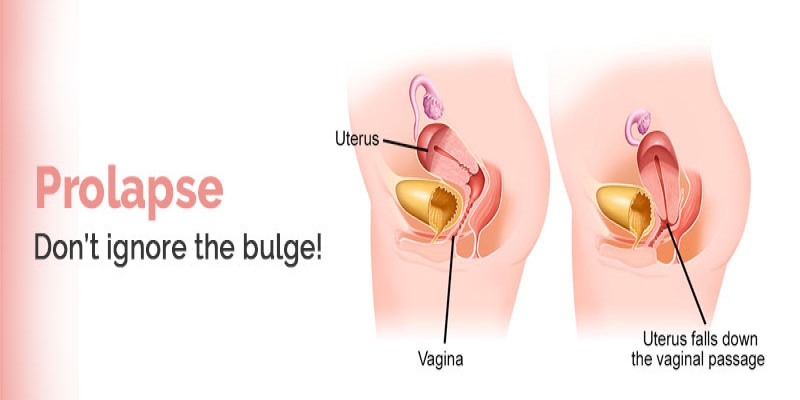
Uterine prolapse occurs when the uterus descends from its normal position into the vaginal canal due to weakened pelvic support tissues. This condition is often caused by factors such as childbirth, particularly multiple or difficult deliveries, which can stretch and damage the pelvic muscles and ligaments. Other contributing factors include aging, hormonal changes during menopause, obesity, chronic coughing, and heavy lifting. Women with a family history of prolapse or connective tissue disorders may also be at higher risk. Symptoms of uterine prolapse can vary but commonly include a feeling of pelvic heaviness or pressure, vaginal bulging, discomfort during sexual intercourse, and urinary or bowel symptoms such as incontinence or difficulty emptying the bladder or bowel.
Diagnosing uterine prolapse typically involves a comprehensive pelvic examination where a healthcare provider assesses the degree of prolapse and any associated symptoms. In some cases, additional imaging or tests may be required to evaluate the extent of the prolapse and the overall condition of the pelvic organs. Treatment options for uterine prolapse depend on the severity of the condition and the patient's overall health. Conservative approaches may include pelvic floor exercises (Kegels) to strengthen the muscles supporting the uterus, lifestyle modifications, and the use of a pessary—a device inserted into the vagina to support the uterus. For more severe cases, surgical intervention may be necessary to repair the pelvic support structures and restore the uterus to its proper position. The choice of treatment is tailored to each individual's needs and preferences, aiming to alleviate symptoms and improve quality of life.
Procedures & Interventions
Strengthening the pelvic floor muscles can help support the uterus and alleviate symptoms of prolapse. Kegel exercises involve contracting and relaxing the muscles that control the flow of urine. Regular practice can improve muscle tone and provide support to the pelvic organs.
Adopting certain lifestyle changes can help manage or prevent worsening of uterine prolapse. These may include maintaining a healthy weight, avoiding heavy lifting, treating chronic coughs, and incorporating fiber into the diet to prevent constipation, which can contribute to pelvic pressure.
A pessary is a removable device inserted into the vagina to provide support to the uterus and prevent it from descending further. Pessaries come in various shapes and sizes and can be adjusted to fit individual needs. Regular follow-ups are necessary to ensure proper fit and function.
For postmenopausal women, hormone replacement therapy may help by improving the elasticity and strength of pelvic tissues. This treatment should be discussed with a healthcare provider to evaluate potential benefits and risks.
-
Surgical options are considered for more severe cases of uterine prolapse or when conservative measures are ineffective. Surgical procedures may include:
-
Hysterectomy: Removal of the uterus, which can completely resolve symptoms but is irreversible.
-
Uterine Suspension or Repositioning: Surgical techniques to restore the uterus to its normal position and reinforce the supporting structures. Techniques may include vaginal or abdominal approaches.
A specialized form of physical therapy focused on strengthening the pelvic muscles, improving pelvic alignment, and addressing any associated symptoms like pain or urinary incontinence.

Strengthening the pelvic floor muscles can help support the uterus and alleviate symptoms of prolapse. Kegel exercises involve contracting and relaxing the muscles that control the flow of urine. Regular practice can improve muscle tone and provide support to the pelvic organs.

Adopting certain lifestyle changes can help manage or prevent worsening of uterine prolapse. These may include maintaining a healthy weight, avoiding heavy lifting, treating chronic coughs, and incorporating fiber into the diet to prevent constipation, which can contribute to pelvic pressure.

A pessary is a removable device inserted into the vagina to provide support to the uterus and prevent it from descending further. Pessaries come in various shapes and sizes and can be adjusted to fit individual needs. Regular follow-ups are necessary to ensure proper fit and function.

For postmenopausal women, hormone replacement therapy may help by improving the elasticity and strength of pelvic tissues. This treatment should be discussed with a healthcare provider to evaluate potential benefits and risks.

-
Surgical options are considered for more severe cases of uterine prolapse or when conservative measures are ineffective. Surgical procedures may include:
-
Hysterectomy: Removal of the uterus, which can completely resolve symptoms but is irreversible.
-
Uterine Suspension or Repositioning: Surgical techniques to restore the uterus to its normal position and reinforce the supporting structures. Techniques may include vaginal or abdominal approaches.

A specialized form of physical therapy focused on strengthening the pelvic muscles, improving pelvic alignment, and addressing any associated symptoms like pain or urinary incontinence.
Team of Excellence
Behind every recovery story at RG Hospitals is a team of exceptional doctors whose passion for healing and innovation continues to transform healthcare and redefine patient outcomes.
Find a DoctorLooking for an Expert
RG Hospitals is proud to be the home of some of the world's most distinguished doctors.

Patient Stories
View AllPatient Testimonial | Commitment To Care
Treated by Dr. Manoj Gupta , RG Stone Hospital, Dehradun
- All Locations
- New Delhi
- Haryana
- Punjab
- Kolkata
- Chennai
- Mumbai
- Goa
- Uttar Pradesh
- Uttarakhand